Blood Types
Blood type is a classification of blood based on the presence or absence of antigens on the surface of red blood cells. ABO blood grouping is the primary blood classification system. The Rhesus (Rh) system is also commonly used in blood typing. Knowing an individual’s blood type is vital for determining compatibility in blood transfusions, as well as for identifying potential blood group incompatibilities between the mother and child during pregnancy.
Antigens
An antigen is any molecule that can trigger an immune response. The immune system checks cell antigens to identify and distinguish one’s own cells from foreign cells and pathogens. When the immune system encounters an unknown antigen, an immune response is triggered against the foreign body. The primary purpose is to protect the body from infectious agents. Antigens on the surface of red blood cells can be chemically identified and used to classify blood types.
Blood Groups
An individual’s blood type is determined by genetic inheritance. For most clinical scenarios, an individual’s blood type is specified by their ABO blood group and their Rh factor.
ABO Blood Grouping
The ABO blood group classifies blood into four main types according to the presence of two antigens—antigen A and antigen B—on the surface of red blood cells. The four types are A, B, AB, and O. Type A has only A antigens on the surface, while type B has only B antigens. Type AB has both A and B antigens, while type O has neither A nor B antigens.
An individual’s immune system creates antibodies against antigens that the individual does not naturally have. For example, a person with type A blood (red blood cells with antigen A) will make antibodies against antigen B. A person with type O blood has neither antigen and will make antibodies against both antigens A and B.
At the population level, type O is the most common blood type and is considered the “universal donor” in blood transfusions due to its lack of antigens. The lack of antigens makes type O red blood cells undetectable by the individual receiving the blood transfusion, so most people can receive type O blood without complications.
Type AB is the rarest blood type and is considered the “universal recipient” due to its ability to receive blood from all other types. This is because a person with type AB blood has an immune system already familiar with the A and B antigens and does not produce antibodies against either. Thus, they can receive blood from type A, type B, type AB, or type O individuals.
Rhesus (Rh) Factor
The Rhesus (Rh) blood group is a classification system used to determine the presence or absence of the Rhesus D antigen (RhD) on the surface of red blood cells. The RhD antigen, also inherited from parents, is found on the surface of red blood cells in 90% of individuals in the general population. Individuals with the RhD antigen on their red blood cells are called Rh-positive (Rh+), while those who do not have the antigen are called Rh-negative (Rh-).
A person’s blood type is written by combining their ABO type with their Rh type. For example, a person might be A+, AB-, or O+, and so on.
Like the ABO blood group system, the Rh system plays a crucial role in determining the compatibility of blood for transfusions. When an Rh-negative individual receives Rh-positive blood, their immune system may produce antibodies against the RhD antigen.
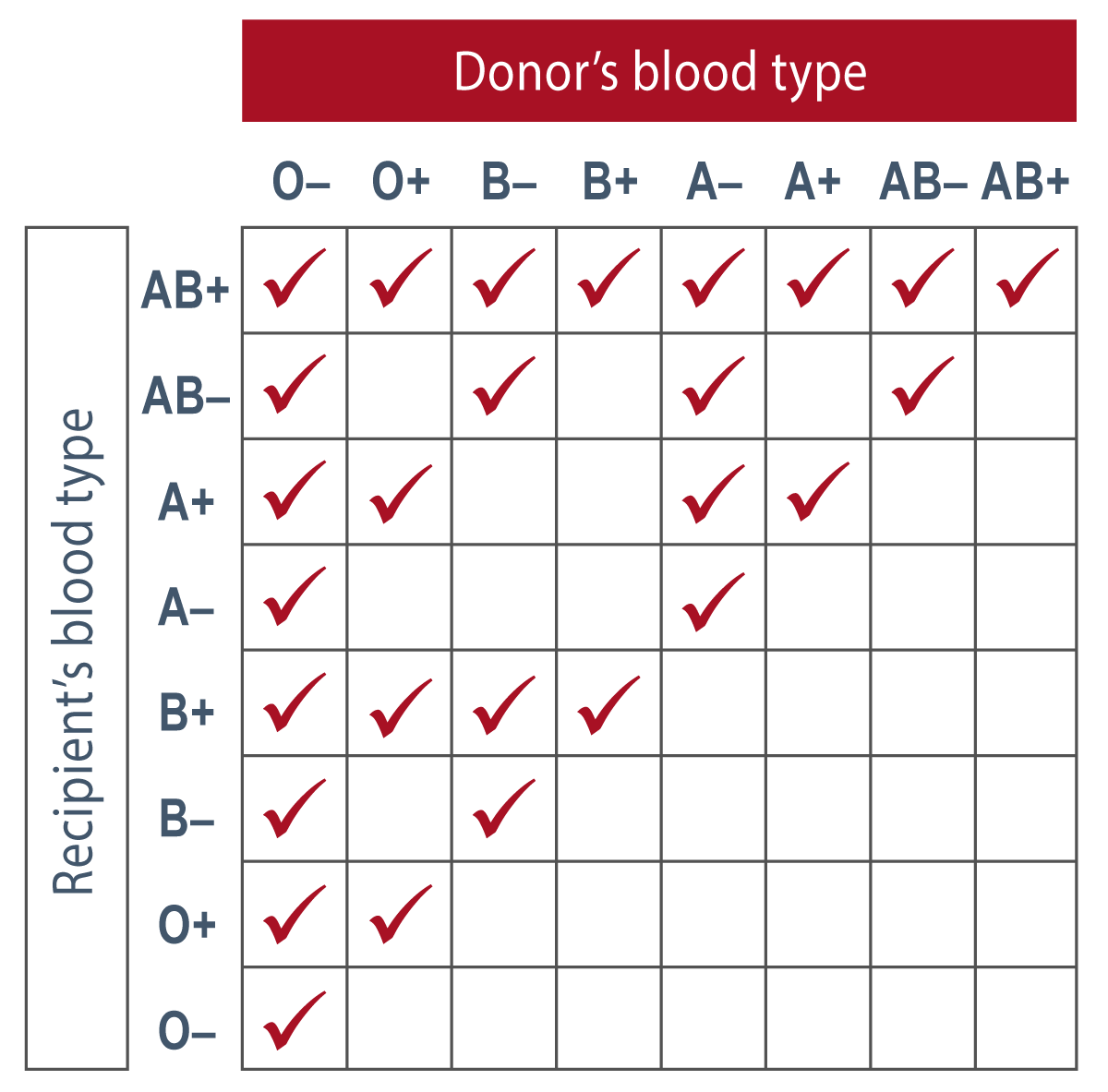
ABO and Rh blood type compatibility table.
Additional Typing
There are more than 40 additional major recognized blood group systems, with over 340 red blood cell antigens recognized by the International Society of Blood Transfusion. Of these systems, Kell, Duffy, Kidd, and MNSs are the most commonly used. They function similarly to the ABO group, with antigens on the red blood cell surface.
Applications
Blood typing is a crucial aspect of modern medical practice that is used in various clinical applications, such as blood transfusions, organ transplants, and preoperative blood compatibility testing.
- Transfusions: Proper matching of blood types between donors and recipients is necessary to prevent potentially fatal transfusion reactions. A mismatch in blood types can lead to the destruction of red blood cells, which can cause serious complications, such as hemolytic anemia, kidney damage, and even death. Blood typing is, therefore, a critical step in the process of safe blood transfusion.
- Organ Transplantation: As ABO antigens exist on the surface of red blood cells and other body tissues, it is preferred to use ABO-matched donors when transplanting organs and tissues to reduce the risk of rejection.
- Pregnancy: Antenatal testing for maternal blood type and Rh factor is essential for assessing the risk of hemolytic disease of the fetus and newborn (HDFN), a potentially devastating or fatal condition resulting from maternal antibodies attacking fetal red blood cells. The modern use of RhoGAM in Rh-negative mothers has significantly decreased the incidence of this disease, but the risk is still present.
- Paternity Testing: Blood typing cannot be used to prove paternity but may be used to rule out paternity in specific cases. Certain blood types can only be inherited with specific combinations. If the mother’s blood type is known, then certain blood types can be ruled out for paternity.
- Disease Resistance/Predisposition: There are certain diseases that are more common in those with a particular blood type. For example, stomach cancer is more common in those with type A blood. Blood type O confers a lower risk of venous thromboembolism due to lower von Willebrand factor. These are just a few examples of the known correlations between blood type and disease risk.
Additional resources:
- Human Blood Groups by Britannica
- Blood Types by The American Red Cross
- Red Blood Cell Antigens and Antibodies by UpToDate
Contributors
- Teresa Roberts, DNP
Reviewers
- Brian Sullivan, MD
Published: March 18, 2023